Doctor on Deck: How Health Workers Can Take a Break
With just a few weeks left in August, Summer is in full swing. Temperatures are high, long nights remain, and celebrations are aplenty. Post-pandemic 'revenge vacations' are still a thing in 2023, and have hit the healthcare industry especially hard. During a health worker shortage, how do you ensure all employees get the time off they need to recharge, while continuing to ensure you have full patient coverage? Patient emergencies can emerge at anytime.
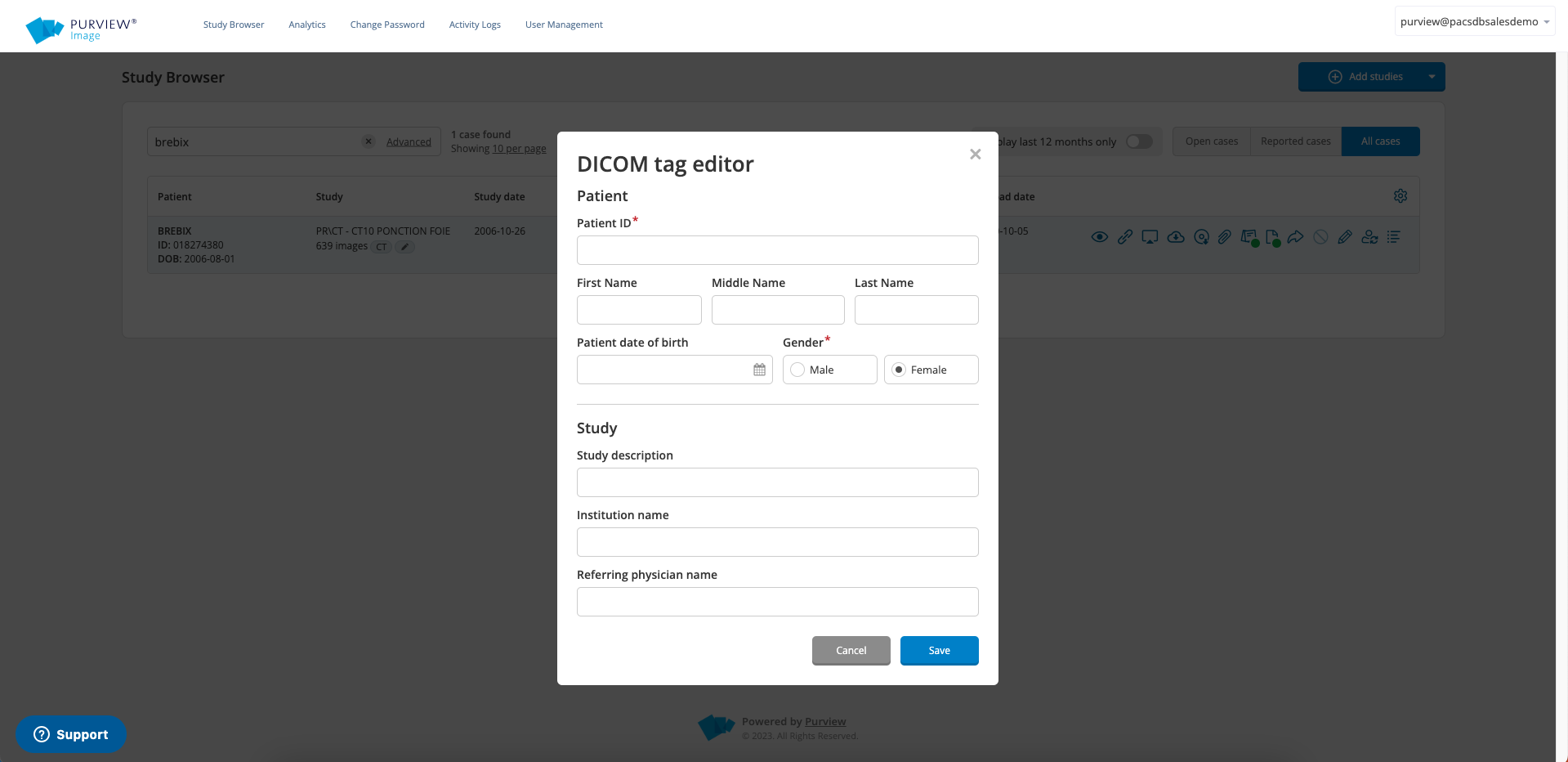
This is where flexible cloud solutions, like Purview Image™ come in. If you need to be available for emergent situations, Image allows you to view patient images on any device and from any location, at anytime. So whether you end up on the beaches of Hawaii, or simply need a staycation, you can opt to stay as connected as you'd like. Perhaps you can even extend your stay, knowing that your patients will be taken care of regardless of where you are?
Let's scroll through a few fun examples while you're soaking in the rays and even try it out for yourself! Have you ever seen an x-ray of a sea turtle, a CT of a dolphin, or iguana?