Why Asynchronous Part 3; Benefits for Payers

In ‘Why Asynchronous Part 1,’ we explored the benefits asynchronous modalities can offer to patients, including improved access, convenience, potential for reduced costs, improved experience, faster throughput, safeguarding of health, and clinical outcomes. Patients have collectively spoken through unprecedented rising demand for telehealth services globally.
In, ‘Why Asynchronous Part 2,’ we discussed the benefits to providers ranging from their ability to better reach and help new patients, to adding revenue sources, improved market positioning, global brand awareness, opportunities for experience, convenience for physicians, reduced physician burnout, and improved retention.
Part 3 of our ‘why asynchronous’ series explores the benefits which asynchronous modalities can offer Payers, ranging from improved data and analytics, to improved throughput, controls, and ultimately lower total healthcare expenditures.
The Challenge of Lowering Healthcare Expenditures 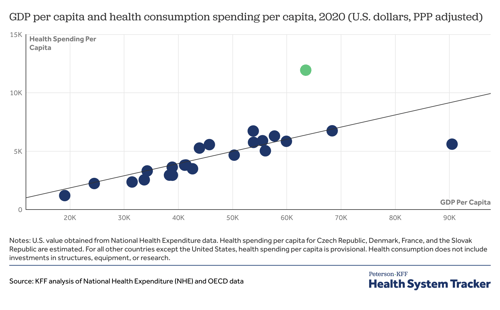
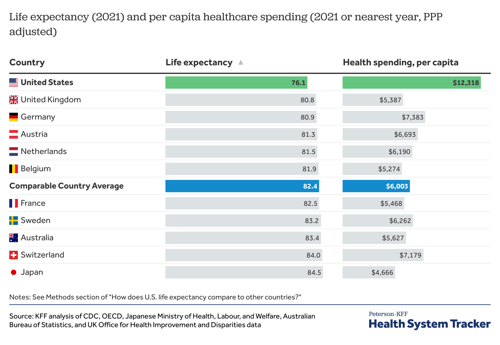
Unfortunately, while we spend quite a bit here in the U.S., we do not necessarily reap the rewards. Life expectancy is noticeably lower in the U.S. compared to many other wealthy countries, who spend less on healthcare per capita. Yet, many individuals travel to the U.S. to receive cutting edge treatment from institutions leading the way in treatments and cures. Creating a competitive environment that spurs innovation tends to conflict with the required environment that provides Medicare for all. So what do we do? The complexity surrounding these issues have become the center of many political platforms. Yet, one bipartisan issue has emerged - telehealth.
Demand for telehealth during the 2020 Covid-19 Pandemic surged, as noted in, ‘Why Asynchronous - Part 1.’ The declaration of the Public Health Emergency (PHE) by the U.S. Department of Health and Human Resources (HSS) in 2020, became the impetus for new telehealth infrastructure. Today, more than three years post-pandemic, many payers have already adopted aspects of telehealth technologies for their own patient populations, including the Centers for Medicaid and Medicare (CMS). The primary benefits?
Increased Competition = Lower Costs
Telehealth market disruption lowers market concentration and increases competition. Further discussed in, ‘Why Asynchronous Part 2,’ the virtual nature of telehealth allows providers to expand well beyond their physical geographic region, a former limitation. This virtual expansion creates exponential opportunity and growth for the healthcare market.
Historically, the FTC has researched and concluded that regions which experience lower market concentration and subsequent higher competition, also experience lower costs. Some studies show that less competitive regions have charged up to 40% more compared to more competitive regions. Building on this argument, the FTC shows that price transparency spurs greater competition through informed consumers and competitors. The insertion of telehealth can be used as a mechanism for supporting these basic benefits of competition theory, resulting in lower costs and more informed consumers able to make better decisions.
Asynchronous is Efficient (self service + convenient + fast + virtual)
In Purview’s experience, asynchronous modalities in particular, are appreciated by physicians due to their flexible nature and efficiencies gained. When appropriate cases are sent through these modalities, physicians do not need to address them in real-time. Instead, they can work them into their day without interrupting their workflow. Some physicians can even work remotely while addressing these cases, an unprecedented benefit. A 2020 UC Irvine study, published by Surgical Neurology International, showed that patients receiving virtual second opinions as opposed to in-person, received them one week sooner on average. Patients get results faster, can move forward with treatment faster, often lowering costs, a win-win.
In addition to the efficiencies gained in throughput, the virtual nature of these appointments removes the need for seeing patients within physical ‘brick and mortar’ facilities. While these expensive facilities are a fixed cost that cannot be removed entirely, telehealth modalities enable administrators to re-purposed the space for patients who do require in-person appointments.
Finally, some asynchronous technologies, like Expert View™, are designed to enable patients to 'self-serve.' This is where patients can handle administrative tasks such as request or upload records, sign forms, connect providers, or communicate all within one system. Enabling patients to self-serve saves on administrative costs, often speeds up the process, and empowers the patient to take control of their health. These technologies also use automation to further enhance efficiencies, rather than relying on human capital, further lowering costs and increasing the speed of delivery.
Opportunity to Improve Controls
Payers implement controls through different mechanisms to ensure that utilization of care is not over-used or abused. In 2019, Health Leaders estimated that the annual cost of over treatment or low-value care was $75.7B - $101.2B. These mechanisms act as a series of checks and balances, such as encouraging second opinions prior to expensive, invasive, and sometimes irreversible procedures, like surgery. The example right, shows a document by CMS, which explains benefits and provides guidance for patients to seek a second opinion before surgery. Many institutes, including the Cleveland Clinic, have published research showing that patients often receive a different or refined diagnosis and treatment plan with a second opinion:
"We have found that 28% of our second opinion consults result in a diagnosis change, while treatment plans are modified in 72% of the patient cases we review.” Peter Rasmussen, M.D., Chief Clinical Officer, The Clinic at The Cleveland Clinic.
Cigna recently shared a white paper showing an average cost savings of $118 per visit by avoiding unnecessary tests during telehealth appointments. Payers can use asynchronous modalities to increase the access and speed of their controls, helping patients to avoid costly treatment that is unnecessary, and instead find answers to get the right treatment faster.
Data & Analytics
Telehealth modalities inherently gather data through the usage of their technologies and platforms, far more than traditional in-person visits. Insurance companies can lower their costs when they can better predict and lower risks. Oscar, Bright Health, and Clover Health are just a few recent insurtech companies to rely on 'big data' and AI to predict and control for risk through targeted preventative care. The goal is to both improve patient outcomes while lowering costs. While these business models have yet to be proven, they show promise. Other insurance companies are already relying on big data for research, modeling, and forecasting. Telehealth modalities will only amplify their potential.
However, as Voltaire reminds us, ‘with great power comes great responsibility.’ Protected Health Information, or PHI, must be safeguarded for patient privacy above all. Payers are in a position to move the needle on health expenditures in the United States, a major problem. But they must also prioritize patient privacy and health outcomes. Strong data governance, ethical guidelines, and accountability will go a long way towards creating our improved healthcare system of the future.
Want to learn more?
Read 'Second Opinions 101,' written in collaboration between Purview and the Advisory Board
Check out Purview's Remote Second Opinion Maturity Model
Read Part 1 and 2 of this series:
Why Asynchronous Part 1; From a Patient's Perspective
Why Asynchronous Part 2; Provider Benefits & Opportunities