Design for Better Health Care - Are We There Yet?
A few weeks ago, the American Telemedicine Association (ATA) held their annual conference in San Antonio, Texas. The show floor was filled with impressive futuristic devices from augmented reality glasses, to home health monitoring technologies, big data products, and more. Executives from Microsoft and Google, Kim Swafford and Bakul Patel, took the stage together, kicking off the weekend with exciting updates and reminders of helpful features that emerged from the pandemic era, such as YouTube’s improved searchability, now including personal stories to help people learn about health conditions. When asked ‘what’s next?,’ panelists joked about the potential for ChatGPT, Kim learning about it from her teenager, but both ultimately settled on describing the buzzword of the weekend, ‘omnichannel.’
An ideal future was painted, where the patient experience was optimized. It was not dependent on a single technology or device, but was more proactive in automatically detecting needs, informing providers ahead of a health event, through an ecosystem of sensors, technologies, and devices. They shared a future that is tailored to each of our individual needs, values, and desires.
This was a great start that left telehealth professionals feeling energized and hopeful, but as the weekend went on, multiple individuals began sharing frustrations with the current state of the industry. There were many complaints from lacking enough resources, to the right knowledge and experience, that the state of policy was in disarray, reimbursement needs to catch up, and the list goes on. The primary looming question could be distilled to - Are we there yet? Well - when will we get there?
When many of the technologies exist to enable the ideal futuristic world described by Microsoft and Google execs, why are we not further in adoption? Tom Lawry urges us to move faster and embrace change in his recently published book, ‘Hacking Healthcare;'
The Time for Intelligent Health Systems is Now - The pandemic taught us much about ourselves and what we expect. It reinforced the importance of healthy citizens and healthy nations. It demonstrated our capacity to change. It also solidified the role AI plays in making things better. These learnings are at the heart of our collective ability to rethink and reboot a system that, without change, is not likely sustainable. (Lawry: pp30)
Hospital leaders and program managers have glimpsed into what our future could look like with improved tools and a little investment. They see a transformed industry that delivers on access to expertise, improved throughput, quality of care, lowered costs, and improved experiences. In the meantime, events titled, ‘Tackling healthcare's challenges shouldn't feel like a game of Whac-A-Mole. 5 healthcare leaders discuss problem solving without trade-offs,’ arrive in our inbox from Becker's.
Can we design our way towards a better future?
One multidisciplinary panel ranged from design professionals to healthcare providers, titled, ‘Designing for the Future of Healthcare Delivery.’ Including Christina Grimes of NBBJ Design, Lygeia Ricciardi of Ada Rose, Geri Baumblatt of Difference Collaborative Alliance, Chris Waugh of Sutter Health - One Medical, and Brian Mullen of the Cleveland Clinic, the panel brought high-level commentary and anecdotes on how we can implement design-thinking to improve the system faster.
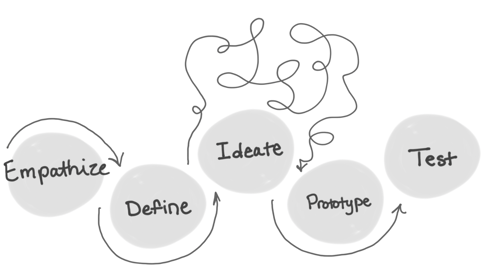 As a designer and instructor for data visualization at the Maryland Institute College of Art (MICA), this topic resonated. The Q&A loosely followed the design process: empathize, define, ideate, prototype, and test, which I have always thought mirrors the scientific process. I was curious how they would motivate the audience to employ design-thinking. The panel began by telling the crowd that each of them are designers, whether they like it or not. We all are creating our future health system, and it's time to get creative.
As a designer and instructor for data visualization at the Maryland Institute College of Art (MICA), this topic resonated. The Q&A loosely followed the design process: empathize, define, ideate, prototype, and test, which I have always thought mirrors the scientific process. I was curious how they would motivate the audience to employ design-thinking. The panel began by telling the crowd that each of them are designers, whether they like it or not. We all are creating our future health system, and it's time to get creative.
Move Fast - But Don’t Break Things
Chris Waugh, a former designer at IDEO, began by reminding us that we can try to move fast, but we can’t break things, unlike Facebook’s early mantra. Human lives are in the balance here. In fact, first we must acknowledge that many aspects of our society are designed to work against improving the state of healthcare in the U.S., using the example of a business selling alcohol whose goals to gain market share are at odds with their consumer's health. The entertainment and retail industries are great at engaging with consumers where they are already consuming content. The healthcare industry can and should learn from this and engage to incentivize healthy habits.
Re-think Existing Systems
Brian Mullen, from the Cleveland Clinic, suggested that there is much untapped value and opportunity in re-thinking established processes. For example, can we leverage texting more often for applicable communications? It’s more direct, secure, skips the need to login to a portal, and best of all, it is also how many people prefer to communicate. Each session embodied this sentiment that the healthcare industry is more resistant to change than any other, and that this problem is reaching its height. If we want a better system, it's time to challenge the status quo.
Human Touch vs Automation
Another panelist suggested that providers create a virtual front door if they have not already, and then ensure it is thoughtfully designed. A well designed virtual front door can improve throughput and patient satisfaction by allowing patients to choose which technologies they are most comfortable using, when appropriate for their case. Automation and self-service can be woven into the experience, improving efficiencies. However, thoughtfully leveraging human connection when it is most valuable is key. This process of intersecting multiple technologies and devices, balancing automation and human touch, and encouraging patients to choose their own path, brings us closer to achieving the omnichannel effect.
Modular Spaces for the Intersection of Physical & Virtual
Perhaps the most interesting portion of the conversation began when Christina Grimes introduced the potential for the intersection of physical environment with the virtual. In addition to home health monitoring, imagine going to the hospital for a procedure where the world's leading expert can observe as if they were there in-person, providing real-time feedback and guidance from anywhere in the world. To a degree this is already happening, but our built environment is not typically designed to facilitate any aspect of this process. Grimes tells us that this is changing, but there is one core challenge. Healthcare settings can take seven years or more to design and build, while technology evolves at lightning speed in comparison. How can we design the built environment with anticipation of where technology will be in seven years? Grimes suggests creating modular solutions that can be readily adapted to future change and innovation.
Shrink the Change - Launch a Pilot
In closing, Chris reminds us that the future is already here, quoting William Gibson, who is famous for saying, ‘The future is here - it’s just not evenly distributed yet.’ No one pointed out the poetic irony of this quote, that Gibson said it more than twenty years ago.
Since we can’t break things, we need to try out and test ideas. We can shrink the change through launching pilots both internally and by partnering with third parties who are willing to take on some of the risk. If health institutions can embrace the idea of pilots, they can figure out how to obtain buy-in, what works and doesn’t work, analyze the results and identify what was repeatable and scalable. With the entire panel nodding, someone mentions that ‘healthcare is starved for creativity.’
---
Collaborative Insights
Finally, in review of the poster submissions, it was impressive to observe the range of applications and problems that telehealth programs were able to solve in just a few short years. It was also interesting to find that many of my own assumptions appeared to be incorrect, most of which surrounded whether remote or in-person engagement was more successful for different types of cases. Although, all of this came with one critical observation - there was not nearly enough data to jump to any conclusions. Each presenter acknowledged this, and was curious to learn from one another. Even amongst competing organizations, there was a spirit of collaboration. If we can more openly share our data and insights - we can get there faster, together.
Want to learn more?
Read 'Second Opinions 101,' written in collaboration between Purview and the Advisory Board
Check out Purview's Remote Second Opinion Maturity Model
![]() Listen to Purview's Webinar
Listen to Purview's Webinar
Delivering the Future of Healthcare - Do Remote Second Opinions Open New Doors?




