Pathology Second Opinions - Look Again
Pathologists are responsible for providing accurate diagnostic information, which guides critical decisions physicians make for their patient. In the United States, 1,752,735 people were diagnosed with cancer in 2019 alone. Globally, the number is an astonishing 17 million. That’s twice the entire population of New York City.
Thus, the accuracy of a pathology read cannot be underscored enough. In 2016, Joann G. Elmore, M.D., Et al., published a study in the British Medical Journal, ‘Evaluation of 12 strategies for obtaining second opinions to improve interpretation of breast histopathology: simulation study,’ which examines the impact of second opinions on the accuracy of breast cancer diagnosis. The results found that 11 of the 12 approaches to obtaining second opinions, improved accuracy. The study states that ‘second opinions will not completely eliminate diagnostic variability, but can significantly improve diagnostic accuracy of interpretation of breast histopathology. Accuracy improved regardless of the pathologists’ confidence in their diagnosis or experience.’
In an accompanying video, Dr. Elmore explains that, ‘diagnosis of Atypia and DCIS can be challenging for pathologists, where there can be extensive variability in the interpretation of the breast tissue. The concern is that an inaccurate diagnosis can lead to under interpretation, resulting in delays in necessary treatment, and an overinterpretation can result in costly and potentially unnecessary therapies.’
This is why many pathologists seek a second read to reach consensus before their final conclusions. Especially complex cases may require a team of specialists and additional tissue samples may be advised. As awareness of these challenges grow, requests for second or third opinions on pathology reports are increasing in demand.
How Do Second Opinions in Pathology Work?
One would think that sending and receiving a pathology sample is a simple task, but anyone in the field will tell you it’s not. Tissue blocks and slides must go through a chain of custody to ensure they are not lost, damaged or attributed to the wrong patient. They must be clearly labeled and carefully and securely packaged.

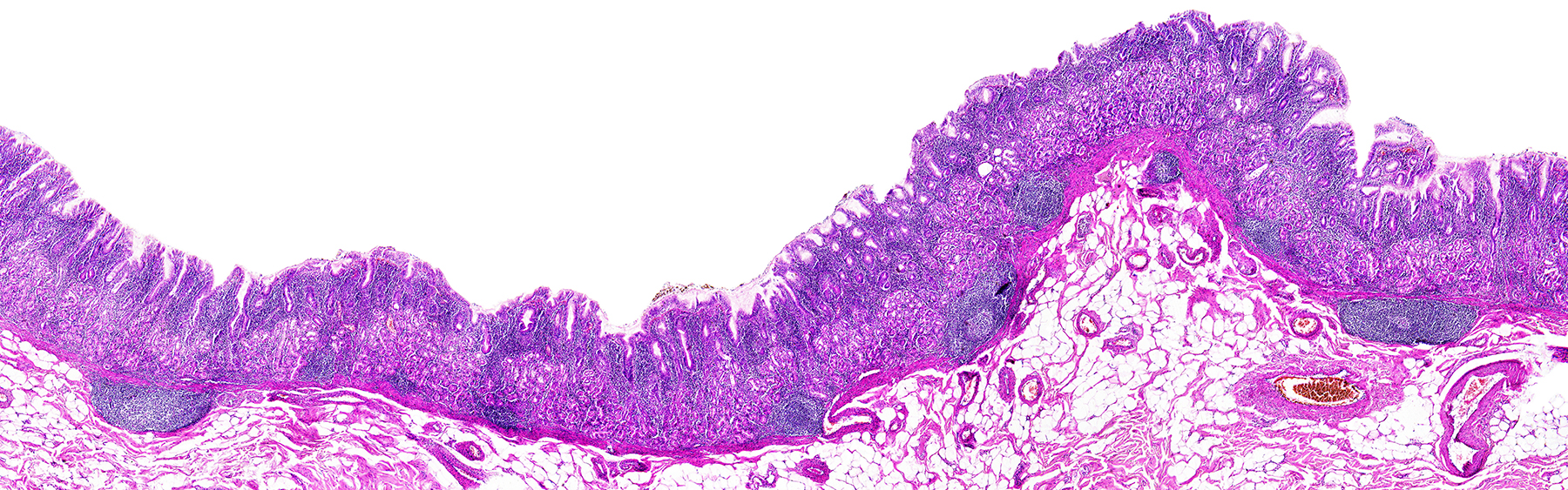
Historically, and still predominantly today, pathology slides are mailed to other locations for confirming reads. While this process is still used today, it comes with a few challenges. For example, pathologists are concerned with matching slides with the correct corresponding cases, which may introduce errors. This is why best practices require clear communication, documentation, and accurate labeling and packaging. A photo of the slide, its packaging, and labeling should be shared with the receiving institution prior to arrival to ensure it is correctly matched (shown left).
Other challenges include time and geography. While some physicians may demand physical slides or tissue blocks, many patients and physicians do not want to wait for this longer, more tedious, process. Additionally, mailing human tissue is not always practical, depending upon where it needs to be sent.
Benefits of Digital Pathology
Digital pathology, as an alternative to mailing physical slides, adds new capabilities that enable greater efficiencies and collaboration across geographies. For example, international patients face many challenges in sending human tissue samples across country borders. Digital pathology circumvents these issues, bringing high resolution scans of the slides to the expert pathologist as fast as the internet can take them.
As noted, multidisciplinary collaboration and additional interpretations are well warranted to ensure accurate diagnosis for the patient. Digital pathology enables easier multidisciplinary collaboration. Tumor board reviews, for example, may be done asynchronously avoiding the need to synchronize schedules of busy clinicians.
Some pathologists prefer the ease and flexibility of digital pathology. Rather than bending over a microscope, these reads can be displayed on a large screen computer, reducing the strain on their neck and back. Others have said that the reduction in errors by using software to match slides to the correct patient through barcodes or unique labeling, helps them to sleep better at night.
Digital Pathology Process
In digital pathology, the second opinion clinician will request that the original institute electronically share the digital pathology images plus any relevant case notes. Once received, the reviewing pathologist can display the image using whatever viewer he or she prefers., [Note, digital pathology formats are not yet standardized requiring viewers to accommodate multiple formats.] The second review can be rendered in a formal written opinion or a consult with the originating pathologist. After this, they will render their opinion in the form of a written report.
Challenges in Digital Pathology
While many pathologists prefer the digital delivery process to mailing slides, there are challenges that need to be addressed. For example, CDs are still a prevalent way to share medical images. So when a request for records is made, sometimes a CD is what the originating institute will send rather than electronic transfer. Much like the process with the physical slides, a CD must also be carefully matched to the appropriate case. [Note, many pathology images are so large they exceed the capacity of a CD and may require a DVD or thumb drive for their physical transfer.]
Some other considerations to keep in mind with digital pathology are file size, viewing software, and viewer requirements. Digital pathology file sizes can be extremely large (double digit gigabytes) and may take some time to upload and view. With time, this pain point will surely become alleviated, as we have seen Moore’s Law play out. Software to facilitate the sharing and standardized viewing of pathology images along with their associated medical records is needed, although today this software is still quite expensive.
While digital pathology is an important step to facilitate access, collaboration, and potentially the most accurate result, the largest challenge is adoption. Humans are habitual, and often retreat in the comfort of old technologies, like CD’s. Perhaps the silver lining of the covid-19 pandemic is that it thrust the healthcare industry into constant creative problem solving, bringing digital solutions to the forefront.
–
Advances and adoption of emerging technologies are enabling collaboration and centralization of expertise beyond anything that has been done before. The pandemic unveiled various disparities in healthcare. Providing access to the right expertise when a patient needs it most is critical to providing the best patient care. Coupled with the fact that a second review may provide a different set of results is becoming more accepted by the medical profession.